The big 3 that I want to discuss this week is unfortunately not about Lebron, Kobe, or Wade. It is the big 3 of low back pain; Disc Herniations, Stenosis, and Degenerative Disc Disease (DDD).
Low Back Pain is a diagnosis that I see most often and will treat. Sometimes low back pain can be chronic. This means it’s been months, or even years that a patient has been experiencing this pain, or it can be more acute due to an accident.
Let’s start with the basics. We will start with what the Big 3 actually looks like, patterns as a patient that you may start to notice, and as a PT what the evaluation process looks like.
Disc Herniations
Disc Herniations… what is a disc? A disc is a structure that lies between two vertebral bodies. Vertebrae’s are the bones that make up our entire spine. The disc is made up of an annulus like material, with the nucleus pulpous in the center. These discs sit between the two bodies and distribute the forces in our spine whenever we move. I always like to thin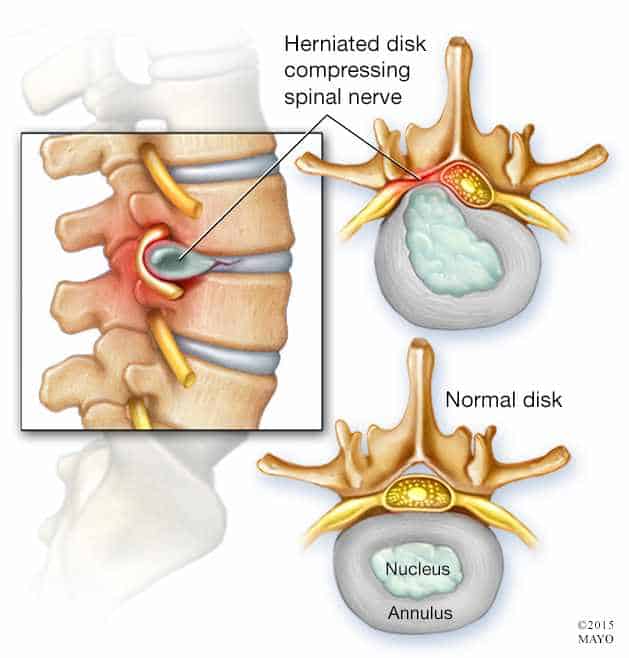 k of the center, that nucleus portion, similar to that of a jelly filled donut. In some instances, not all, whenever the donut is squished the jelly will ooze out of it. Sometimes that jelly or the nucleus will push on the spinal cord, causing numbness and tingling in your legs, or what we like to call in medicine radicular symptoms. Now it’s important to understand these discs will not always be jelly filled donuts. In fact, on average between the ages of 30-35, the discs will become dry and the least likely cause of low back pain.
k of the center, that nucleus portion, similar to that of a jelly filled donut. In some instances, not all, whenever the donut is squished the jelly will ooze out of it. Sometimes that jelly or the nucleus will push on the spinal cord, causing numbness and tingling in your legs, or what we like to call in medicine radicular symptoms. Now it’s important to understand these discs will not always be jelly filled donuts. In fact, on average between the ages of 30-35, the discs will become dry and the least likely cause of low back pain.
Now you’re probably saying “well my MRI shows that I have a disc herniation”. Well that can absolutely be valid. However, this may not be the root cause of your low back pain, given factors like age and more often these discs tend to heal on their own. So how do we rule in a true disc herniation? Well as a patient you may start to notice sitting for prolonged periods of time tend to aggravate you, but walking or standing feels better, and of course that annoyance of what feels like your legs are just constantly asleep. With those reports, the PT will typically look at how well you can touch your toes, extend backwards, move side to side, and rotate. Then the PT will check muscle strength, sensation, and reflexes. One specific test in particular is called the Straight Leg Raise (SLR). This involves the passive lifting of the leg, should aggravate back pain, and increase that numbness and tingling.
Spinal Stenosis
Now, spinal stenosis, similar to that of disc herniations will cause those radicular symptoms. What you will start to notice is walking or standing tends to aggravate your symptoms, but feel relief when you’re sitting. Typically a patient is at least 48 years old or older, and numbness and tingling is in both of their legs. More recently, research has found you may start to notice that numbness and tingling in your groin. For the PT the same exam occurs as disc herniations. But, new research has found that a 2 stage Treadmill test can be a good indicator to rule in stenosis.
Degenerative Disk Disease
 Last but not least Degenerative Disk Disease (DDD) which is synonymous with having arthritis in our spines. One conversation with my Clinical Instructor (CI) truly clarified DJD and hopefully as you read this, you’ll have a better understanding as well. “Arthritis is like having wrinkles in your spine”. We often associate wrinkles with age, as how arthritis develops with age. Wrinkles in our skin are typically not painful, therefore the wrinkles in our spines don’t have to be painful either. Arthritic changes will absolutely show up on an imaging exam, and it can be daunting to hear, but does not mean that your back pain is hopeless. Again, with a thorough exam, we need to locate if there is any weakness, or mobility deficits and treat them as such.
Last but not least Degenerative Disk Disease (DDD) which is synonymous with having arthritis in our spines. One conversation with my Clinical Instructor (CI) truly clarified DJD and hopefully as you read this, you’ll have a better understanding as well. “Arthritis is like having wrinkles in your spine”. We often associate wrinkles with age, as how arthritis develops with age. Wrinkles in our skin are typically not painful, therefore the wrinkles in our spines don’t have to be painful either. Arthritic changes will absolutely show up on an imaging exam, and it can be daunting to hear, but does not mean that your back pain is hopeless. Again, with a thorough exam, we need to locate if there is any weakness, or mobility deficits and treat them as such.
So what’s the takeaway from this? Many different sources can attribute to low back pain. A thorough exam can rule in or rule out causes. And like any other body part low back pain is treatable!