For a very long time, we in medicine have worked under what we call the Biomechanical Model of Pain. That is that the belief that the pain receptors in X structures have been stimulated by damage, and therefore must be causing local pain. If we fix the structure, we fix the pain.
Except it has not been working very consistently. People will sometimes undergo multiple so called mechanical fixes to a region without resolution of pain. People will come in and we cannot find a damaged structure in the region to fix, so we determined the pain must not be real. Essentially, the model was failing to explain entire populations in pain, and we as a field have been blaming the populations and not the model.
Thankfully, research over the recent years has been shining a lot of light on this, and we have learned a great deal about pain that completely changes how we view it, and in turn has created some very exciting prospects for how we can treat it!
 Let’s start with what we’ve learned is entirely wrong: the human body does not actually have “pain receptor” nerves at all! It turns out the original researchers who labeled these nociceptors never called them that to begin with, it was a simplification for young students to begin to grasp the concept that got out of hand! Nociceptors, by original definition, detect “possibly damaging stimulus to the region.” Essentially, they are a warning system that triggers our brain to pay more attention to something so we can determine if it is of immediate danger that requires a response.
Let’s start with what we’ve learned is entirely wrong: the human body does not actually have “pain receptor” nerves at all! It turns out the original researchers who labeled these nociceptors never called them that to begin with, it was a simplification for young students to begin to grasp the concept that got out of hand! Nociceptors, by original definition, detect “possibly damaging stimulus to the region.” Essentially, they are a warning system that triggers our brain to pay more attention to something so we can determine if it is of immediate danger that requires a response.
This actually makes a lot of sense when we think about it, because pain is not always triggered by sensation through the nociceptors anyway, sometimes excessive mechanical load through nerves like our golgi tendon organs can also trigger this response, and sometimes pain arises without any physical damage present, like post exercise pain (formerly associated with “muscle tearing” but now debunked thankfully!).
So what this means is that all pain is actually rooted in the brain’s interpretation of a variety of nerve inputs into it! When we get any input into our brain, it needs to determine what it means, and if it might indicate danger so our body can appropriately respond! Now, the brain’s response is a conditionable thing, we see this in reaction times and psychology all the time. But what we’ve discovered is that this is also true in regards to pain. This is where people with different “tolerance to pain” come in. It’s not that they have less sensitive pain receptors, it is often that their systems simply have a different interpretation of what they feel is “dangerous” vs “not dangerous.”
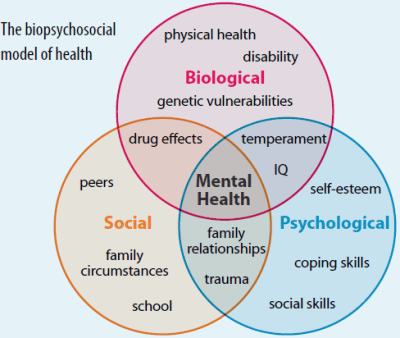
So what influences when our brain decides in input is noxious or not? Turns out, A LOT. And this is where the Biophyscosocial model comes in actually. Biological input, sensory input from vision, nociceptors, mechanoreceptors, auditory receptors, even smell (ever smell burning flesh? Immediate trigger right?) is first sent to the brain. The brain then compares this experience with previous experiences it has had. Is it more or less intense than previous ones? Or, is it entirely unfamiliar? Is it something we are familiar with by proxy of another person we’ve witnessed? Was it sudden or expected? Is the situation it arose from controlled or hazardous? All of these questions are processed almost instantaneously and a determination is made!
 So you can actually see how the psychosocial aspect plays into pain heavily. Those of us who are conditioned to feel that any loud crack might mean a fracture are more likely to have a brain that wants to protect us from that, and we will have a more drastic pain response than those who feel that cracking and creaking are just a normal part of their lives and know they’ve rarely had pain from it before. This all comes from conditioned experience, or lack thereof, to extrapolate data and determine appropriate response. But this also means that bodies under higher stress, a response in the body that originates from the perception of danger to the homeostatic balance of the body, are more likely to trigger a more noxious interpretation of input as the situation that input arose in was already in a stressed body.
So you can actually see how the psychosocial aspect plays into pain heavily. Those of us who are conditioned to feel that any loud crack might mean a fracture are more likely to have a brain that wants to protect us from that, and we will have a more drastic pain response than those who feel that cracking and creaking are just a normal part of their lives and know they’ve rarely had pain from it before. This all comes from conditioned experience, or lack thereof, to extrapolate data and determine appropriate response. But this also means that bodies under higher stress, a response in the body that originates from the perception of danger to the homeostatic balance of the body, are more likely to trigger a more noxious interpretation of input as the situation that input arose in was already in a stressed body.
So how does this change how we treat pain? Does it mean we stop addressing the nociceptors and possible damage in the body? Absolutely not!! Those pieces of the puzzle are still major players in the game, and we cannot ignore that fractures, wounds, and burns are truly dangerous damage, they’re the entire reason we have the pain system to make sure we don’t further injure that area! However, it means that we also need to look deeper past the physical damage and its severity to understand pain. Has the stress that affected the severity of that pain resolved or is a patient still struggling under the mountain of medical bills and difficulty paying them because their injury put them out of work? Well we need to work on that stress too, otherwise their brain will have a very hard time turning off a warning system! Did the cause of injury put them in a serious situation that makes the body feel generally unsafe like a traumatic accident? You can bet a fair amount of money that if their brain is still reactive to those things their pain is too!
What does this mean for people who don’t have physical damage but still have pain? People like chronic injuries that have technically healed years ago but still hurt, or people with fibromyalgia, does this help them? Quite a bit! This understanding that damage did not have to occur for us to experience real pain can help us try and figure out what and why the body perceives things as dangerous, and help address those roots and try and improve the quality of life for everyone in pain, regardless of if I can fix something physical or not!