Gout is a type of arthritis that develops in individuals with high levels of uric acid in their blood. It is a common type of arthritis and causes intense pain, swelling, and stiffness in a joint, typically affecting the joint of the big toe.
The CDC reports over 8 million Americans were affected by gout between 2007 and 2008. This type of arthritis occurs in about 4% of American adults which is about 6 million men and 2 million women.
Stages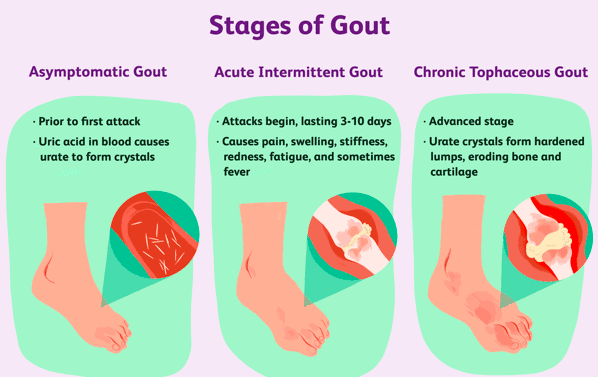
There are multiple stages of gout.
Asymptomatic Hyperuricemia
This period comes before the first attack of gout. There are no symptoms but the blood uric acid levels can be high and crystals start to form in the joint. These crystals may deposit in the tissue causing slight damage. Though treatment is not required, people with this type of gout may be advised to address any factors that contribute to the uric acid build up.
Acute Gout
This stage occurs when the uric acid levels spike or the crystals in the joint are messed with, triggering the attack. The sudden attack or “flare” normally goes away in 4 to 10 days. Attacks or “flares” can be triggered by stress, alcohol, drugs, and cold weather. Though some people may never experience a second attack, 60% of people will have another within the year. Overall, 84% of people may have another within 3 years.
Interval Gout
This is the period between acute gout attacks. Though there is no pain, the gout is not gone. Low-level inflammation could be damaging joints between attacks. During this time is when to begin managing your gout with medications or a lifestyle change. Doing so can help prevent chronic gout and future attacks.
Chronic Gout
When your uric acid levels continue to stay high over a multiple number of years, chronic gout develops. A person only gets to this stage if they go without treatment for around 10 years. It is highly unlikely a person who is receiving proper treatment would ever get to this stage.
Risk Factors
Age and Gender. Men produce more uric acid than women do. However, women’s levels of uric acid do approach those of mens after menopause.
Genetics. If you have a family history of gout, the likelihood of your condition developing increases.
Lifestyle Choices. Consuming alcohol interferes uric acid leaving the body. Also eating a high-purine diet increases the amount of uric acid in the body.
Lead Exposure. Some cases of gout have been linked to chronic lead expos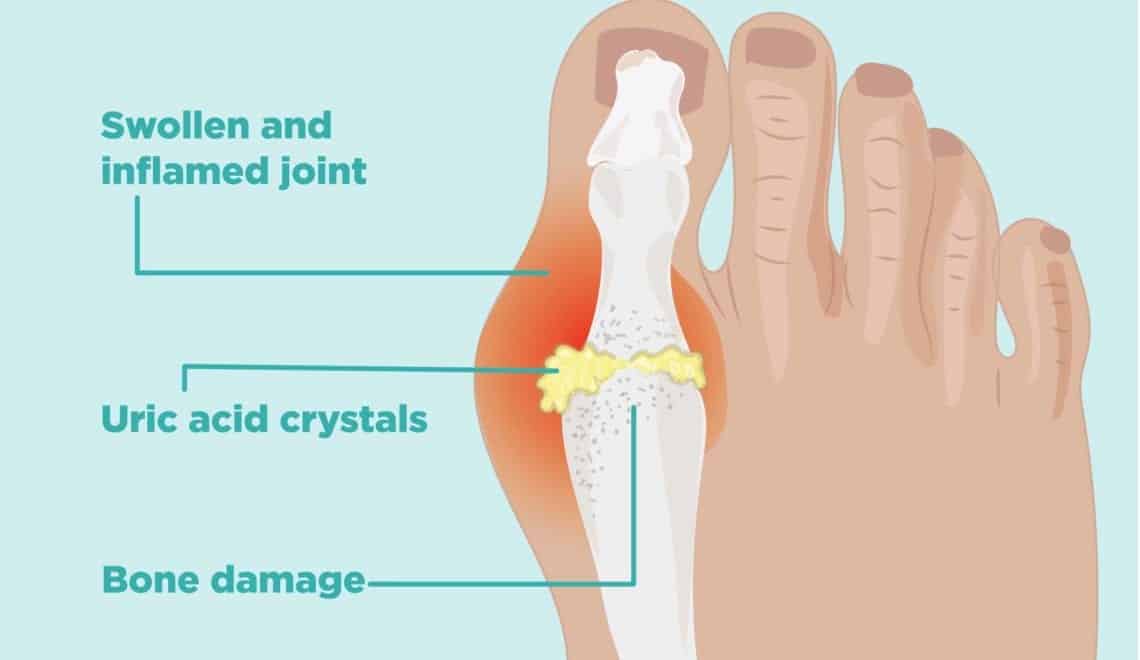 ure.
ure.
Medications. Taking certain medications can increase the levels of uric acid in the body. These medications include diuretics and drugs containing salicylate.
Weight. Gout is increased by being overweight because there is more turnover of body tissue. This means there is more production of uric acid as a metabolic waste product. Also, higher levels of body fat increase the levels of systemic inflammation as the fat cells proceed pro-inflammatory cytokines.
Recent Trauma or Surgery increases the risk of gout.
Other Health Problems. This includes renal insufficiency and other kidney problems that may reduce the body’s ability to effectively remove waste products which in return can lead to elevated levels of uric acid. High blood pressure and diabetes are also associated with gout.
Diagnosis
Based on a review of your medical history, a physical exam, and symptoms a doctor will be able to diagnosis you. More than likely your doctor will base your diagnosis off the description of your joint pain, how often you experience intense pain in your joint, and how red/swollen the area is.
Treatment
If gout is not treated it can lead to arthritis. It may also lead to your joint being permanently damaged and swollen. The plan your doctor decides to use for treatment depends on your stage and severity. Medications used to treat gout can work in a day or so, relieving pain and decreasing inflammation. Medication can also lower uric acid levels which helps prevent future attacks from occurring.
Besides medications, your doctor may recommend a lifestyle change. This can include losing weight, exercising more, quit smoking, better eating habits, and reducing your alcohol intake.
Lastly, physical therapy may be an option. A PT can assess your affected joint and prescribe range of motion, stretching, and strengthening exercises that help maintain the maximum function of the joint.



